Eczema
Introduction
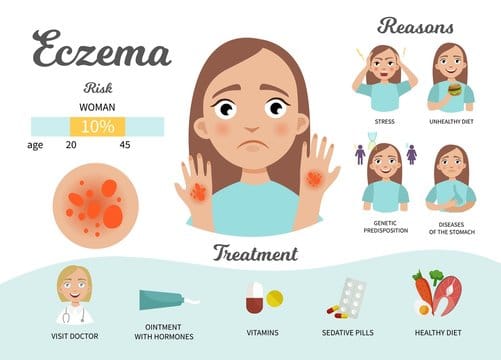
A prevalent skin condition that results in red, itchy, and inflamed skin patches is called eczema, also known as atopic dermatitis. Eczema is a persistent illness, which means that it can last for a very long time and may recur occasionally. Although it can happen to people, children are the most frequently affected.
Although the precise cause of eczema is unknown, it is thought to be a result of a mix of genetic and environmental factors. In addition to certain triggers like tension, dry skin, or exposure to irritants or allergens, people with eczema may have a genetic predisposition to the disease.

Pathophysiology
The exact pathophysiology of eczema is not fully understood, but it is believed to involve a complex interplay of genetic, immunological, and environmental factors. One of the key features of eczema is a defect in the skin barrier, which allows irritants, allergens, and microbes to penetrate the skin and trigger an immune response. The skin barrier is made up of layers of cells and lipids that help to retain moisture and protect against external threats. In people with eczema, this barrier is disrupted, making the skin more susceptible to damage and inflammation. In addition to the skin barrier defect, eczema is also characterized by an overactive immune response. In response to triggers such as allergens or irritants, immune cells in the skin release inflammatory mediators such as histamine, cytokines, and leukotrienes, which cause redness, itching, and inflammation. Genetic factors are also thought to play a role in the development of eczema. Several genes have been implicated in the condition, including genes involved in the skin barrier function, immune function, and inflammation. Environmental factors such as dry skin, harsh soaps, and certain foods or allergens can also trigger or exacerbate eczema symptoms. Stress and hormonal changes may also play a role in some cases.
Signs and Symptoms
The symptoms of eczema can vary in severity and may include:
- Skin that has red, inflamed areas
- An itchy or tight sensation in the affected region
- Dry or flaky skin
- In severe instances, the skin may begin to ooze or crunch.
- Over time, brittle or thickened skin
- Skin discoloration or pigmentation alterations
- Tiny, raised bumps that, if scratched, could release fluid
- Skin that is delicate and is easily affected by certain substances or products.
How do Dermatologists treat Eczema?
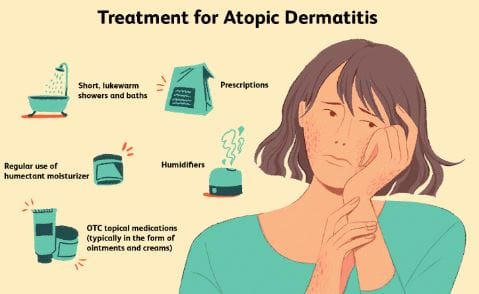
Dermatologists use a variety of treatments for eczema, depending on the severity of the condition and the individual’s symptoms. Some common treatment options include:
- Use moisturisers frequently to prevent dryness and itching and to keep the skin moisturised.
- Topical corticosteroids. They are offered in a variety of concentrations and formulations, including creams, ointments, and lotions.
- Topical calcineurin inhibitors: These drugs reduce inflammation by preventing the immune system’s reaction in the skin.
- Systemic corticosteroids: Oral or injectable corticosteroids may be recommended in severe eczema cases to lessen body-wide inflammation.
- Immunomodulators are drugs that target particular immune cells that are implicated in the inflammatory response.
- Antibiotics: If a bacterial infection results in the eczema, antibiotics may be recommended.
- Phototherapy: This method of reducing inflammation and itching includes exposing the skin to particular light wavelengths.
Dermatologists might also suggest dietary changes, the use of mild skin care products, and the practise of stress reduction methods in addition to medical treatments for eczema.